Genesis
In a previous post, we talked about COVID Watch. Watch depended on self-reported dyspnea i.e. patient self-reported if their breathing was worse. While this worked and continues to work well, physicians in the ED were faced with a tougher problem. They had patients who showed up and while they perhaps could be considered for admission, their O2 sat numbers were either good or borderline. For these patients, they faced the tough challenge of deciding between admitting them (especially given bed shortages) and discharging them without having an adequate means of monitoring them. While these patients could have been (and some were) enrolled into Watch, there was a clinical baseline of O2 sat readings that should and could drive re-admissions. The need of the hour was to get these patients pulse oximeters, train them on their use, get them to report these readings on a daily basis and depending on relative drops in O2 sat readings, bring them back into the ED for admission. This team was led by Dr. Kathleen Lee (ED physician), Lauren Hahn (Innovation Manager) and Neda Khan (Application Specialist, W2H) along with numerous personnel from the various ED departments.
Operational implications
COVID Pulse was a quick follow-up to the Watch project. The biggest challenge that needed to be addressed was the sourcing and procurement of Pulse Oximeters. Kat was able to identify a qualified source in Atlanta and managed to push that through the procurement process quickly. In addition, there was distribution of the devices to each of the participating EDs that needed to be considered.
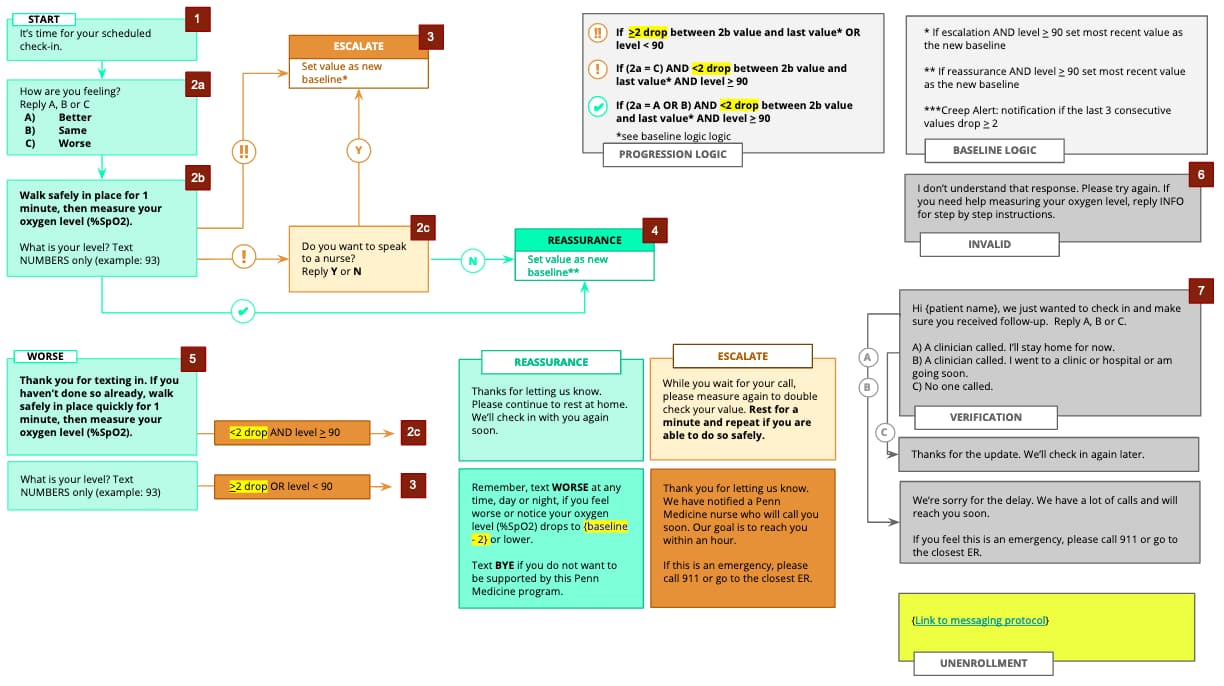
The logic for the program was iterated upon considering input from multiple clinical stakeholders. The more or less final version is shown below. As you can see, it takes into account:
- Rapid relative drops: If the relative drop from the discharge SpO2 reading is =>2 (this number was increased to 3 subsequently), then an alert would be generated and an escalation sent into the EPIC in-basket pool.
- Creeping drops: If the patient SpO2 gradually 3 or more points drops over time, this also generates an alert and an escalation.
- Absolute baselines: If the patient SpO2 drops below 90, W2H generates an alert and an associated escalation.
Note that these are self-reported SpO2 levels. Associated training material needed to be created and provided to both the clinician and the patient for educational purposes.
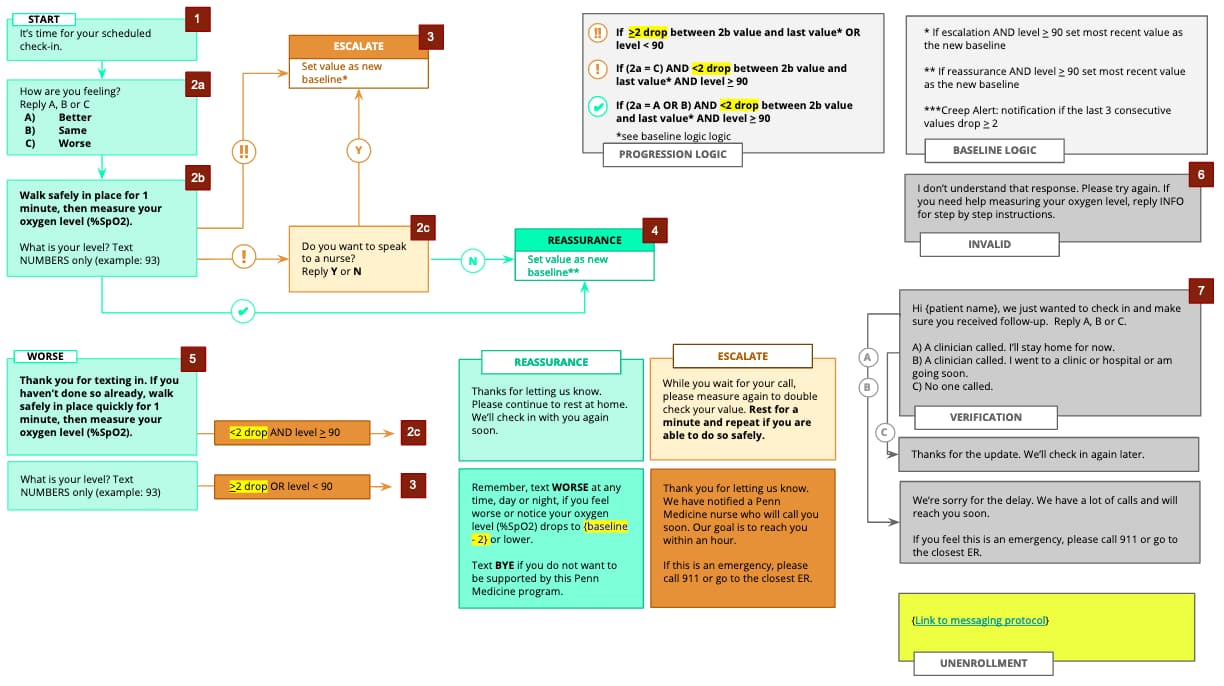
The program leveraged the same personnel who received the escalations from the Watch program. The escalations generated by this program contained language that identified the patient as being part of the Pulse program and also included details such as discharge SpO2, last SpO2 and relative drop. This allowed the nurses to confirm details before recommending a course of action. The algorithm also had logic built in that would ask the patient (if safe) to retake the SpO2 reading if it seemed erroneous.
Ramping up and numbers
We knew upfront that this program was very different from Watch. It has pre-requisites (a device to be handed over and educated on, for one) and was targeted at a very specific patient population. The program launched in April, 2020. To date, the program has supported 531 patients.
We discussed the Watch program in our earlier post. The one thing we kept coming back to was to understand the difference between self-reported and objective measures of dyspnea and the subsequent care provided. As mentioned earlier, this led to the PCORI award to not only understand this difference but also evaluate the difference in how this addressed racial disparities.
More to come
The PCORI Pulse / Watch program has completed it’s enrollment numbers in record time (4 months) and we are in the process of analyzing the data. We hope to report on that soon.
Hope you found this post useful. Please feel free to drop us a line via the Contact link below and we’ll be happy to discuss this more with you. Look for part 6 of this series next week.